T1D Guide
T1D Strong News
Personal Stories
Resources
T1D Misdiagnosis
T1D Early Detection
Research/Clinical Trials
Here’s How the One Big Beautiful Bill May Impact People with T1D
When it comes to politics, it’s tough to know who to trust, especially when both sides are touting they are right. Such is the case with President Trump’s new One Big Beautiful Bill (OBBB). While the law promises to cut government healthcare costs, some analysts warn it could also tighten Medicaid rules, potentially leaving low-income patients, including those with type 1 diabetes (T1D), with coverage gaps and higher costs.

The American Diabetes Association (ADA) urged the Senate to reject the bill, citing that federal funding for diabetes research and public health infrastructure was at risk. They also highlighted the fact 92% of adults seeking Medicaid are already working or unable to work due to illness or caregiving, warning that the new requirements and frequent recertifications will lead to “reduced enrollment and eligibility, disrupting access to medications, insulin, and care for people with diabetes and prediabetes.”
To better understand the pros and cons of the bill and what advocacy steps you can take to ensure your rights are protected, read on!
The OBBB, which passed by the House of Representatives on May 22, 2025, and the Senate on July 1, 2025, may impact the following:
Market Place Changes
In healthcare terms, marketplace changes refer to fluctuations in the way insurance plans are sold, priced and regulated. These changes can include premium adjustments, eligibility rules, and coverage levels.
Some foreseeable changes to the existing Affordable Care Act (ACA) marketplace could lead to higher premiums, more complex enrollment practices and reduced tax credits, making it harder for T1Ds to afford insurance.
Changes to Medicaid
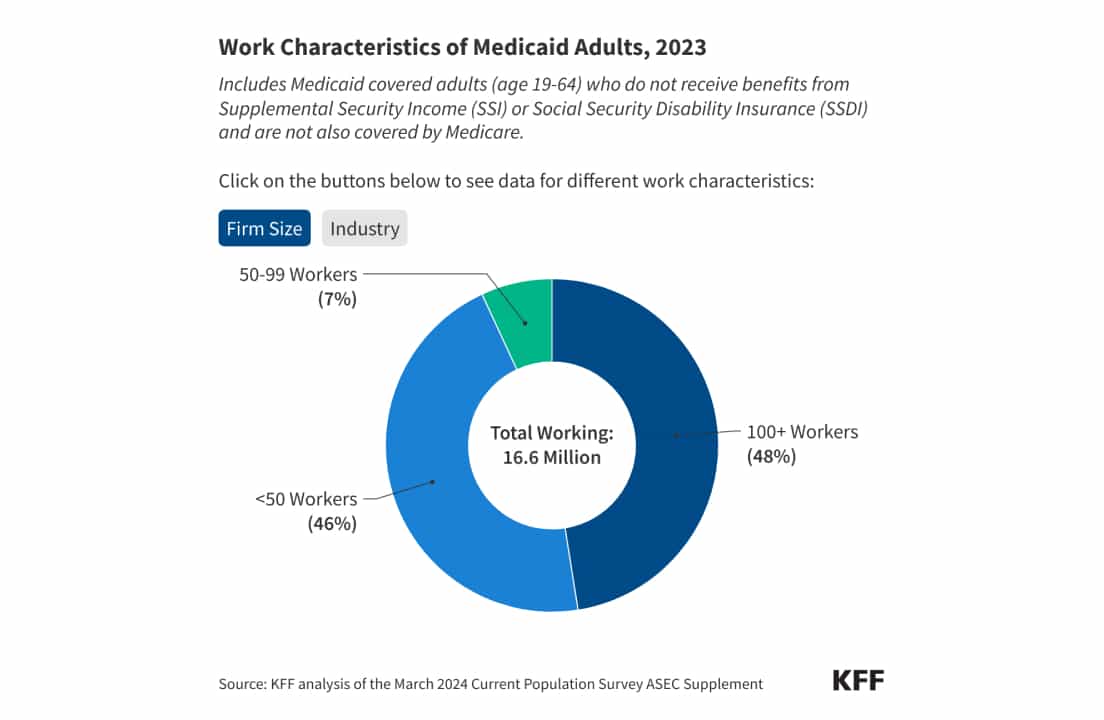
According to the Kaiser Family Foundation (KFF), the OBBB added more work requirements to those seeking Medicaid. Adults on Medicaid must now complete 80 hours/month of work, volunteering or education, unless they qualify for an exemption (like disability or caregiving). People with type 1 diabetes and other chronic illnesses may lose coverage if they can’t meet these criteria.
The ADA notes the work requirement takes effect December 31, 2026—three years earlier than initially planned.
Medicaid Cuts & Facility Closures
The OBBB has set up $1 trillion in Medicaid funding cuts over the next 10 years. The Washington Post reports the shortfall may hurt healthcare facilities, especially in rural areas, forcing clinics and hospitals to shut down or reduce their hours. Additionally, T1Ds may experience less options with access to endocrinologists, diabetes educators and insulin supplies.
As of June 2024, approximately 78.6 million people in the U.S. are enrolled in Medicaid and the Children’s Health Insurance Program (CHIP); these cuts could result in millions losing coverage.

Coverage Gaps
Moving forward, Medicaid could cover fewer months of past medical bills (from three months to one to two months), increasing the risk of uncovered costs after emergencies. Moreover, hospitals may raise costs for insured patients to make up for Medicaid funding losses.
Also, emergency hospitalizations for diabetes complications like diabetic ketoacidosis (DKA) may not be fully covered if patients aren’t enrolled or approved in time.
Increased Costs and Complications
Policy changes like eliminating automatic reenrollment and eligibility may result in higher out-of-pocket costs for people with T1D. More paperwork and red tape may result in fewer doctor appointments and wellness checks, increasing the risks of long-term complications like nerve damage, heart disease and vision problems for those with T1D.
Will the OBBB Lower Insulin Costs?
Despite Trump’s talk about lowering healthcare drug costs in the U.S., there are no direct insulin price caps in the OBBB. Additionally, there is a real concern that these changes may lead to higher insulin prices for insured patients, as a means to offset the Medicaid cuts.
Also, the ADA has expressed concern over aligned cuts in the Supplemental Nutrition Assistance Program (SNAP), which could worsen food security, a critical factor in diabetes management.
PROS of the Bill
While most advocacy groups cite the risks of the OBBB for Medicaid recipients, here are a few possible pros for individuals with T1D.
More Transparency
The OBBB’s transparency provisions apply more to hospital services and providers, not insulin pricing. Moving forward, hospitals and clinics are required to list prices for services, medications, and devices.
This change could help T1Ds compare diabetes supply costs, including insulin pumps and continuous glucose monitors, when paying out-of-pocket expenses or with high-deductible plans.

Regulations for Pharmacy Benefit Managers
Pharmacy benefit managers (PBMs), the go-betweens who negotiate drug prices, will now be required to disclose their negotiated prices and rebates upfront. This will hopefully expose hidden costs and reduce backdoor deals that inflate insulin prices. If implemented, these changes could lead to greater patient savings.
Future Generic Drug Access
The bill includes measures to speed up FDA approval of biosimilar generic drugs, which could benefit those with type 1 diabetes. Competition in the drug industry could drive prices down for diabetes medications and insulin, but this is a long-term possibility.
State Flexibility
Each state may be able to regulate its own Medicaid waivers, customizing Medicaid programs for chronic conditions, like T1D. Which is why speaking out to state representatives and letting your voice be heard is crucial.
What You Can Do
With these changes set to take effect at the end of 2026, now is the time for advocacy and preparation. Here are some tips to help navigate the possible changes to coverage and expenses.
- Stay current on Re-Enrollment
- Monitor your state’s Medicaid plan.
- Document medical limitations and keep records of health challenges you may face.
- Engage with state lawmakers and community members
- Hold state representatives accountable who voted in favor of this bill.
- Seek help from the ADA or Breakthrough T1D, which offer legal advocacy support.
- Get involved with local and federal organizations to fight for diabetes rights.
Understand Your Rights
While the One Big Beautiful Bill pushes for greater transparency, it may negatively impact individuals with type 1 diabetes, especially those on Medicaid.
With risks to healthcare coverage, it’s essential to understand your rights and protect access to care, not only for yourself, but for those less fortunate. Stay informed, get involved with grassroots organizations and speak up to safeguard your liberties.


.webp)





.webp)
.jpg)
.jpeg)
.jpg)
.jpg)

.jpg)


.jpg)

.jpg)
.jpg)



.jpg)



.jpg)




.jpg)

.jpg)



.jpg)

.jpg)




.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)

.jpg)
.jpg)
.jpg)



.jpg)
.jpg)
.jpg)

.jpg)

.jpg)














.jpg)


.jpg)







.webp)











.webp)














.webp)