T1D Guide
T1D Strong News
Personal Stories
Resources
T1D Misdiagnosis
T1D Early Detection
Research/Clinical Trials
Type 3c Diabetes: How Ric Peralta Turned a Rare Diagnosis Into Advocacy and Awareness
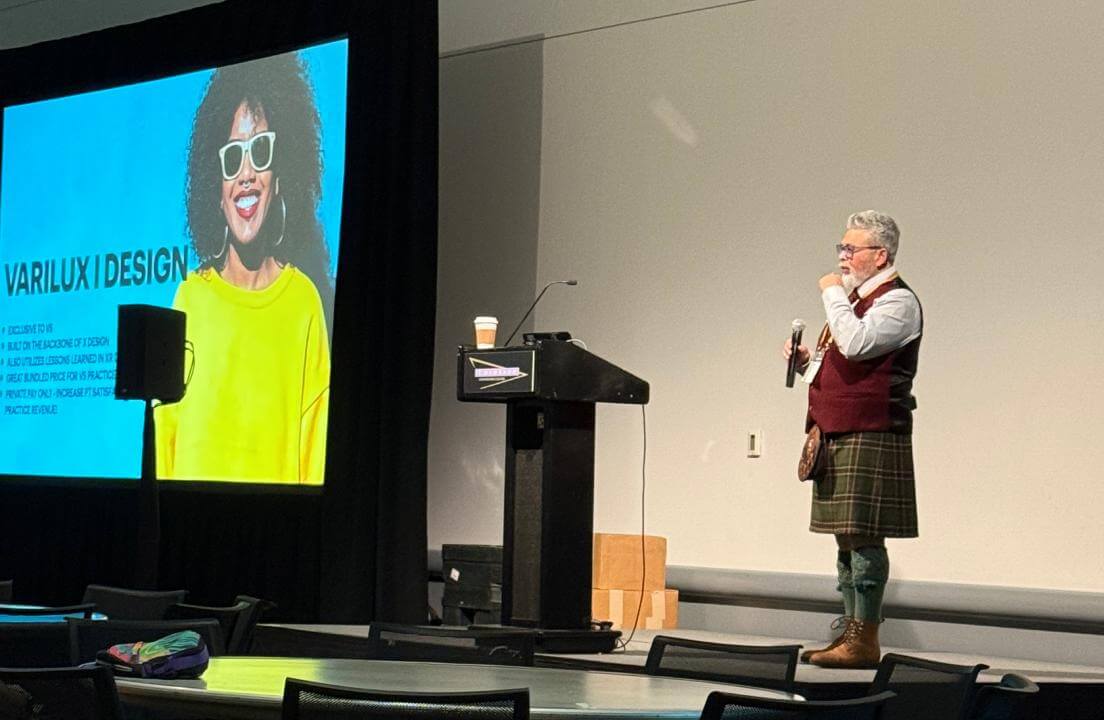
Type 3c diabetes, also called pancreatogenic diabetes, is a rare form of diabetes caused by damage to the pancreas and is often misdiagnosed as type 2. For optician, consultant, and Healthy Sight Ambassador Ric Peralta, the diagnosis came suddenly after a medical crisis in 2003.

Today, he manages the condition with advanced diabetes technology, unwavering support from family and friends, and a passion for educating others. His journey spans from life-threatening hospital stays to national conferences, and from finding resilience in recovery to sharing his story publicly.
The Day Everything Changed: The Start of Ric’s Type 3c Diabetes Journey
On the morning of Aug. 2, 2003, Peralta was on his way to work at an optometry office in California. Saturdays were busy—just the doctor and Peralta holding down the fort. He stopped for breakfast, knowing breaks would be scarce.
One bite of a donut was all it took. Pain shot through his abdomen so sharply it took his breath away.
“I thought maybe I had food poisoning or the stomach flu,” Peralta said. “It was a rough day at the office, running to the bathroom over and over.”
Two days later, Peralta still couldn’t keep down even water. He went to the doctor and was put straight into an ambulance. He wouldn’t leave the hospital for three months.
Severe acute pancreatitis had ravaged his pancreas. By the time he was discharged, part of his pancreas and his gallbladder were gone—and he was living with type 3c diabetes.

What Is Type 3c Diabetes?
Type 3c diabetes, also called pancreatogenic diabetes, develops when the pancreas is damaged or partially removed. The damage affects both endocrine function, which produces insulin and glucagon, and exocrine function, which makes the digestive enzymes that help break down food.
Common causes include chronic pancreatitis, pancreatic surgery, pancreatic cancer, cystic fibrosis, or a physical injury to the pancreas. In some cases, it can also develop after long-term alcohol use or gallstones that block pancreatic ducts.
“It’s not the same path for everyone,” Peralta explained. “But the end result is the same—we all have a missing pancreas.”
Because it stems from pancreatic damage, type 3c diabetes is often misdiagnosed as type 2 diabetes (T2D). That’s because blood sugar patterns can look similar at first. But unlike type 2, it isn’t driven mainly by insulin resistance, and unlike type 1, it isn’t an autoimmune condition.
People with type 3c often require insulin therapy to replace what their pancreas can no longer make, as well as pancreatic enzyme replacement therapy to help digest food properly. Without those enzymes, the body can’t fully absorb nutrients, which can lead to weight loss, fatigue, or gastrointestinal symptoms.
Experts say early recognition and accurate diagnosis are key. Treating type 3c as type 2 can delay proper care and increase the risk of complications such as malnutrition or severe hypoglycemia.
Life After the First Surgery: Adjusting to Type 3c Diabetes
The 2003 hospitalization was only the beginning. Over the years, Peralta underwent three more abdominal surgeries: a hernia repair, spleen removal, and another partial pancreatic resection. Today, he estimates he has about one-third of his pancreas left.
“I think it produced a little insulin for about five or six years after that first surgery,” he said. “But now, I don’t think it’s doing anything.”
Peralta used pancreatic enzymes for seven years to help digest fats. Over time, they seemed less effective, so he stopped taking them.

His condition mirrors type 1 diabetes (T1D) in many ways: no natural insulin or glucagon production, daily glucose management, and reliance on diabetes technology.
But there are key differences that make living with type 3c more unpredictable.
“If I have more than about 45 grams of fat in a day, my body just rejects the food after that,” he said. “That can lead to dangerous lows because I’ve taken insulin for a meal my body never absorbed.”
Finding the Right Tools for Managing Type 3c Diabetes
For the first six or seven years, Peralta managed his diabetes with multiple daily injections using a sliding scale. Eventually, conversations with others living with diabetes led him to try the InPen smart insulin pen.
In 2021, he switched to the Omnipod insulin pump. Around the same time, he discovered the Dexcom continuous glucose monitor (CGM) after a patient told him about it.
“I went to their website right then and there and applied,” Peralta said. “Two weeks later, I had my first Dexcom G5. My A1C dropped three points in the first three months. I was catching all these hidden peaks and valleys I never knew about.”
Today, the pump and CGM work together to keep him in range most of the time. But technology isn’t perfect. Peralta recalls a day when his pump was leaking and his blood sugar hovered around 270 for hours.
“You have to learn to take a breath and ride out the bad days,” he said. “Stress just makes it worse.”
Challenges Beyond Blood Sugar
Managing type 3c isn’t just about numbers—it’s also about navigating a medical system that doesn’t always recognize the diagnosis.
“I’ve had endocrinologists tell me they wouldn’t give me insulin if there was a shortage,” Peralta said. “Insurance paperwork doesn’t even have a spot for type 3c.”
Travel can be another obstacle. Peralta often flies to teach at state eye care conferences. At airports, he’s sometimes met with confusion when asking for preboarding.
“I’ve taken to saying I have type 3c diabetes,” he said. “It confuses them enough that they just say ‘OK.’”
A Love Story in the Middle of Recovery
Just seven months after he left the hospital for the first time, Peralta met the woman who would become his wife—thanks to Star Wars, Harry Potter, and Disneyland.
A lifelong Star Wars fan, Peralta had camped out for every film since 1999 at the TCL Chinese Theatre in Hollywood, spending weeks on the sidewalk with fellow fans.
“So, yeah, I’m a BIG GIANT NERD,” he laughed. “There’s more than one reason I’m called the Optical Jedi.” The nickname stuck, and today it’s both his social media handle and the name of his website, OpticalJedi.com.
His future wife was friends with one of those “line members” and joined the group to see Harry Potter and the Prisoner of Azkaban on opening night.
“We spent a couple of hours in line together,” Peralta recalled. “The next day we went to a costume exhibit at the Motion Picture Academy, and the day after that we went to Disneyland.”

It was love at first sight. And it came at a time when Peralta was still adjusting to his new reality—his surgical drains had been removed only a week earlier.
Advocacy Through Eye Care
Peralta has worked in eyecare for 36 years and has been named a Healthy Sight Ambassador twice. He uses his own visible diabetes devices to start conversations with patients about the link between diabetes and vision health.
“Transitions lenses with blue-light and UV protection can help reduce the risk of macular degeneration,” Peralta said.
“We already deal with a higher risk of diabetic retinopathy. Anything we can do to lower other risks is worth it.”
He stresses that even people without vision prescriptions should have annual eye exams. The retina contains the smallest visible blood vessels in the body, and imaging can reveal early signs of high cholesterol, high blood pressure, and more. For people with diabetes, Peralta recommends retinal imaging every six months.
Support Systems
At home, Peralta’s wife and daughter track his numbers through Dexcom’s sharing feature. His coworkers know to listen for pump or CGM alarms, and his network of friends in the eyecare field check in during conferences.
Just this morning, his wife noticed something was off before he left for work. “She took one look and said, ‘Are you OK?’ I’d had a small low after eating lunch late, but I knew I was trending up again.”
The couple’s adventures include road trips through multiple national parks—seven in just 10 days on one occasion. The Peralta family is also Disney park fans and can often be found at Disneyland.

Finding Strength in the Struggle
Living with type 3c has taught Peralta more than just how to manage a chronic condition.
“I was terrified when I was first diagnosed,” he said. “I thought my life was over. But nothing could be further from the truth. The opportunities and connections I’ve had because of diabetes—I wouldn’t trade them.”
His advice to the newly diagnosed: “Yes, it’s scary. We take medicine that can save us or kill us if we take too much or too little. But it teaches you to listen to your body in a way most people never do.”
Raising Awareness
Type 3c accounts for an estimated 1% to 9% of all diabetes cases, yet it is often misdiagnosed as type 2. Early and accurate diagnosis can lead to better treatment, improved quality of life, and fewer complications.
For Peralta, the condition is more than a medical label—it’s part of his story, and by sharing it, he hopes more people will recognize the signs of type 3c diabetes and receive the care they need.


.jpeg)





.webp)
.jpg)
.jpg)

.jpg)
.webp)

.jpg)
.jpg)
.jpg)
.jpg)


.jpg)

.jpg)


.jpg)
.jpg)


.jpg)

.jpg)
.jpg)

.jpg)
.jpg)

.jpg)
.jpg)
.jpg)
.jpg)
.jpg)

.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)

.jpg)
.jpg)
.jpg)

.jpg)
.jpg)


.jpg)
.jpg)
.jpg)
.jpg)
.jpg)














.jpg)


.jpg)













.webp)





%20(1).png)




.jpeg)










.webp)