T1D Guide
T1D Strong News
Personal Stories
Resources
T1D Misdiagnosis
T1D Early Detection
Research/Clinical Trials
Infant Type 1 Diabetes and Early Detection: What Parents Need to Know About Screening
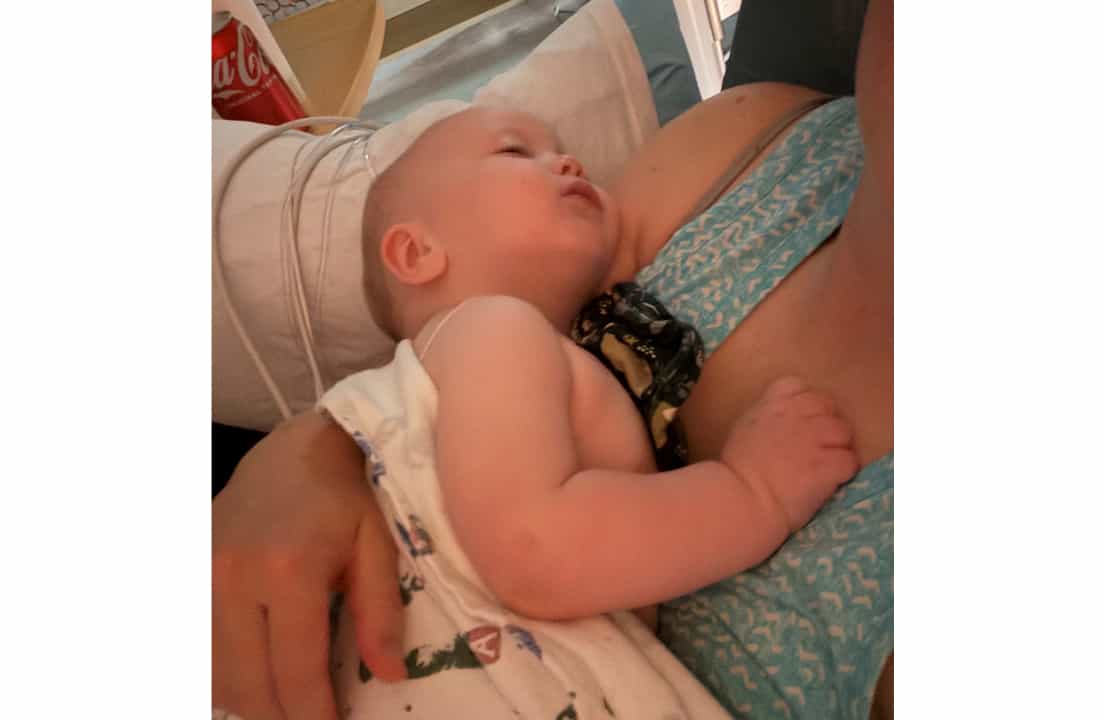
In April 2025, Kylie Grimes and her husband faced every parent’s worst nightmare. Their six-month-old son, Noble, was rushed to the hospital, dangerously ill with what doctors first suspected was pneumonia. After three days on oxygen, he was stable enough to go home. But three weeks later, they noticed something was very wrong.
.jpg)
A baby in crisis: How DKA led to a diagnosis of infant T1D
Noble was unusually clingy, glassy-eyed, and lethargic. He vomited again and again, falling asleep between episodes. His breathing became heavy, slow, and labored. Grimes, a mother of four, knew this wasn’t normal — even with her experience raising three older children. She rushed him to the ER. Doctors considered meningitis and other conditions, but not diabetes.
Noble was severely dehydrated, and it took several attempts and painful pokes before the medical team was able to start an IV. Once the IV was in place, they tested his blood sugar. The number flashed: 576 mg/dL. Noble was in severe diabetic ketoacidosis (DKA). He was moved to the pediatric intensive care unit (PICU). It took a full day for him to regain his alertness. Noble spent eight days in the hospital as doctors worked to stabilize him.
An infant in DKA, a child at risk, read on to hear this family’s story that shows why parents need to know about type 1 diabetes (T1D) screening and early detection.
Type 1 diabetes in infants: Why treatment looks so different
Type 1 diabetes is already a lifelong and demanding condition. In infants, it presents challenges that are rarely taught and often misunderstood.
At first, the nurses caring for Noble didn’t know how to manage such a young patient. His endocrinologist eventually stepped in, retrained the staff, and assigned him to a smaller team of nurses who could handle his care.
Much of the standard diabetes education also didn’t apply.
Grimes was told to follow the standard 15/15 rule — give 15 grams of carbs for a low, then recheck in 15 minutes. But Noble was only seven months old. He couldn’t drink juice, and even if he could, that amount would overwhelm his body.
Infants like Noble follow very different guidelines for insulin treatment and low blood sugar corrections.
Insulin must be diluted, and lows are corrected with only a fraction of the amount that would be given to an older child or adult. What might save one child could harm another. Breastfeeding became a lifeline. Grimes learned it raised his blood sugar gently and predictably. “Breast milk has saved him from lows many times,” she said. Noble now takes diluted Humalog and Lantus, with a blood sugar target goal of 150 to 250 mg/dL.
A second diagnosis: Stage 2 type 1 diabetes in a 6-year-old child
What’s more, as the family adjusted to Noble’s diagnosis, another shock came. Grimes’s six-year-old daughter, Goldie, cut her hand and asked if she could check her blood sugar with her brother’s meter. To Grimes’s surprise, the number read 416.
She called her endocrinology team, and they advised her to take Goldie to the hospital immediately. Testing confirmed stage 2 type 1 diabetes. Out of five autoantibody markers, Goldie was positive for four.
Because she was only six, Goldie did not qualify for Tzield, the first FDA-approved therapy shown to delay the onset of stage 3 type 1 diabetes. The drug is approved only for patients ages eight and older. While Tzield does not reverse the disease, studies show it can delay the need for insulin in patients up to three years.
Just 63 days after Noble’s T1D diagnosis, Grimes’s second youngest child was also facing the condition.
Goldie stayed in the hospital for one day. She was sent home with a continuous glucose monitor (CGM) but no insulin. For now, her family and medical team closely monitor her readings. She has since progressed and is now positive for all five autoantibodies. She will soon undergo an oral glucose tolerance test.
Unlike Noble, who nearly lost his life to undiagnosed diabetes, Goldie’s diagnosis came early. Her parents now walk the line between constant vigilance and preparing for what lies ahead.

Why screening for type 1 diabetes in children matters
Before Noble’s diagnosis, Grimes had never heard of TrialNet, an international research program that screens relatives of people with type 1 diabetes. Her endocrinologist recommended testing the entire family. Both parents and their three other children were screened. Her two older children and both parents tested negative. Only Goldie tested positive, confirming what they already feared.
For Grimes, the decision to screen was not easy, but it was necessary. She explained: “I’m still in a daze about my life, but I sit here and process it. Yes, I am grateful for early detection, because if I can save even one mother from watching her children slip into DKA, I will scream from the mountaintops for screening. That’s the only reason I choose to screen my other kids.”
When she talks to other parents, she finds mixed opinions. Some want to know, others do not. But she says one thing is always the same: fear.
“Fear of the test coming back positive, and fear of sitting helplessly as your child slowly becomes insulin-dependent. Neither road is pretty. Both are heavy with fear. But for me, I’d rather know. I’d rather prepare. I’d rather face what’s coming than always live wondering.”
Stages of type 1 diabetes in children explained
Type 1 diabetes does not appear overnight. Researchers now recognize it develops in three stages, often years before symptoms appear:
- Stage 1: Two or more type 1 diabetes autoantibodies are present. Blood sugar is still normal, and there are no symptoms.
- Stage 2: Autoantibodies are present, and blood sugar levels begin to rise. Still, there may be no obvious symptoms yet.
- Stage 3: Clinical diagnosis. Blood sugar is high enough to cause symptoms such as thirst, frequent urination, weight loss, or dangerous DKA. Insulin is required for survival.
Screening can help families detect the condition in stages 1 or 2, often before it becomes a dangerous emergency.
The five autoantibody tests doctors use for type 1 diabetes screening
Screening looks for five key autoantibodies that signal the immune system is attacking the pancreas:
1. GAD65 (glutamic acid decarboxylase antibody)
2. IA-2 (insulinoma-associated protein-2 antibody)
3. IAA (insulin autoantibody)
4. ZnT8 (zinc transporter eight antibody)
5. ICA (islet cell antibody)
A positive result on two or more of these tests means a child is at high risk of developing type 1 diabetes. This is why TrialNet and similar programs are so important — they allow families to monitor and prepare before the condition reaches stage 3.
The emotional toll: How type 1 diabetes affects families and siblings
The medical side of type 1 diabetes is only part of the story. The emotional impact on Grimes’s family is immense.
Goldie has watched her baby brother endure endless pokes and pricks, insulin doses, and emergencies. One night, as Grimes read her messages of encouragement from other parents online, Goldie started to cry.
“I’m scared to get sick,” she told her mother.
Her 11-year-old sister, Ellie, comforted her. Ellie wants to become a diabetes educator when she grows up. She promised Goldie, “You won’t be alone. I’ll help take care of you and Noble.”
The Grimes family leans on one another constantly. Their strong faith and close bond help them face the hardest days together. The children encourage each other, their parents reassure them, and their faith gives them hope that they are not walking this road alone.

The family is also seeking therapy for their children. They want to help them process the constant fear, the talk of death, and the anxiety that comes when Noble has dangerous lows.
Does early detection of type 1 diabetes prevent heartbreak?
Grimes has now seen both extremes. She has watched the life drain from her baby in a matter of hours due to undiagnosed type 1 diabetes. She has also watched another child enter stage 2 slowly, giving the family time to prepare.
She says early detection does not take away the heartbreak. Sometimes it feels harder, because you know what’s coming. But she believes the knowledge can save lives.
“Neither road is easy. But I’d rather know. I’d rather prepare.”
Finding support: How community and faith carry families through
Since sharing her story on Instagram, Grimes has connected with parents around the world. Each family has a different journey, but they all carry the same burden: helping their children live with type 1 diabetes.
Some parents choose screening. Others do not. But Grimes says the common thread is the same — trepidation.
Still, there is also hope. Support from strangers has lifted her family. Goldie smiles when she hears encouraging messages read aloud by her mom. Even in the hardest moments, connection makes a difference.
Faith has also carried the Grimes family through. Grimes says their belief in God gives them strength on the darkest nights and gratitude on the better days. Their faith, combined with the love they have for one another, grounds them when fear feels overwhelming.
Why this family’s story highlights the importance of screening for type 1 diabetes
The Grimes family’s experience highlights the importance of screening and awareness. Too often, diabetes is not considered in infants or young children until it’s too late.
Programs like TrialNet, along with knowledge about the stages of type 1 diabetes, provide families with an opportunity to prepare.

Early detection may not prevent the condition, but it can prevent life-threatening emergencies like DKA.
For Grimes, that is reason enough.
The future of type 1 diabetes screening and awareness
Two type 1 diabetes diagnoses in two months changed the Grimes family forever. But through fear, vigilance, strong faith, and deep love for each other, they are finding their way forward.
Grimes’s message is simple yet urgent: parents need to be aware of screening. Doctors need to test blood sugar sooner. Families deserve the chance to prepare before a crisis strikes. Because sometimes, awareness is the difference between life and death. And sometimes, what carries a family through is the unshakable support of each other and the strength of their faith.


.jpeg)





.webp)
.jpg)
.webp)
.jpg)

.jpg)
.jpg)
.jpg)

.jpg)
.jpg)

.jpg)
.jpg)
.jpg)
.jpg)

.jpg)

.jpg)


.jpg)
.jpg)
.jpg)

.jpg)
.jpg)


.jpg)
.jpg)


.jpg)
.jpg)
.jpg)
.jpg)
.jpg)


.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)

.jpg)
.jpg)

.jpg)
.jpg)
.jpg)

.jpg)
.jpg)


.jpg)

.jpg)
.jpg)

.jpg)


















.jpg)



.jpg)














.webp)








.webp)