T1D Guide
T1D Strong News
Personal Stories
Resources
T1D Misdiagnosis
T1D Early Detection
Research/Clinical Trials
Doctors at UI Health Performed the First Islet Transplant with Lantidra
On August 26, 2025, a 69-year-old man, Edward Augustin III, from Illinois, received the first islet cell transplant with Lantidra, an FDA-approved cell therapy that utilizes donor pancreatic islet cells. Within one week, he was able to stop taking daily insulin injections.

What is Lantidra?
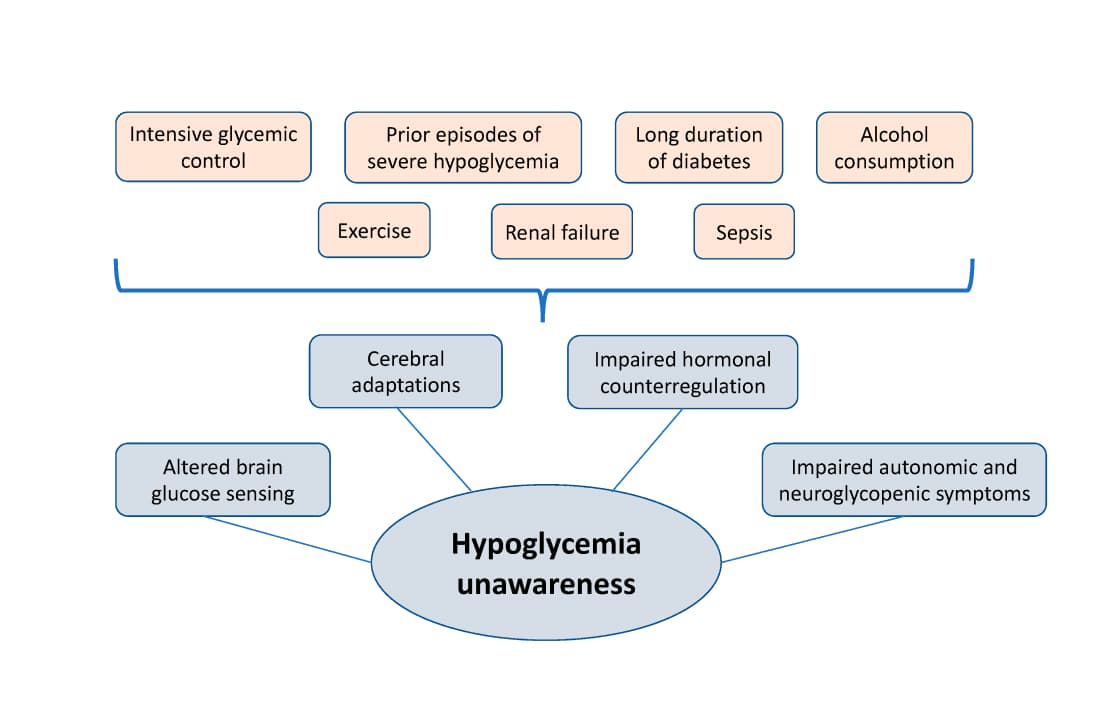
T1D Strong has been closely following Lantidra, a cellular therapy for adults with type 1 diabetes (T1D) who experience severe hypoglycemia (low blood sugar) or hypoglycemia unawareness.
The American Diabetes Association (ADA) reports that of the 1.4 million people in the U.S. living with type 1 diabetes, an estimated 280,000 to 560,000 experience hypoglycemia unawareness.
Hypoglycemia unawareness is a dangerous complication that increases the risk of severe low blood sugars, which in turn can cause seizures, loss of consciousness, accidents, and even death. Additionally, over time, recurrent episodes also raise the risk of long-term complications such as cardiovascular events, kidney disease, and vision problems.
How it Works
The treatment uses islet cells from deceased donors and infuses them into the patient’s liver via the hepatic portal vein. The transplanted functioning cells can produce insulin, the hormone produced by the pancreas that regulates blood sugar levels.
Who Can Try It
The Lantidra treatment is only available right now for T1D adults who:
- Have been insulin-dependent for more than five years
- Are unable to achieve target HbA1c levels despite intensive diabetes management
- Those who experience repeated severe hypoglycemia or hypoglycemia unawareness
The Catch: Immune Suppression
Things to consider with this type of treatment include the use of immunosuppressive medications to prevent the body from rejecting transplanted donor cells. Immunosuppression drugs carry risks (infections, side effects, and cancer risks).
Despite the use of immunosuppressive drugs, it’s still considered a success because some participants no longer require daily insulin injections, and they are protected from life-threatening low blood sugar.
Additional Limitations:
- Other side effects reported by clinical trial participants include nausea, fatigue, and diarrhea.
- There is also a risk of adverse reactions from the infusion procedure.
- Donor cells are in a limited supply.
- Eligibility is limited to adults with long-standing type 1 diabetes (T1D) who meet the severe hypo or hypo-unawareness criteria.
Lantidra 2025 Transplant
Lantidra received FDA approval for its islet cell therapy in June 2023, with UI Health as one of the first centers to offer it as a standard treatment outside of a clinical trial.
The Illinois man, Augustin, who was diagnosed with T1D at age five, experienced severe hypoglycemic episodes, making him an ideal candidate for the infusion. In 2011, he received two experimental islet cell transplants as part of a clinical trial at UI Health, which led to him being insulin-independent for 12 years. The transplant was performed under the Investigational New Drug (IND) framework. Augustin relapsed in 2023 and needed external insulin again.
Now, for the first time, doctors have performed a second islet cell transplant. However, this one is FDA-approved, using Lantidra, a specific formulation of donor islet cells manufactured by CellTrans, Inc.
.jpg)
Transplant surgeons Dr. Pierpaolo Di Cocco, Dr. Enrico Benedetti, and Dr. Lorenzo Gallon at UI Health performed the operation.
Why the Transplant Matters
“This is the first time in the United States that an islet transplant was no longer experimental, rather an FDA-approved medical procedure,” said Dr. Benedetti, head of the Department of Surgery at UI Health.
“The advantage of an islet transplant is that there is no age limit. We would never dream of doing a pancreas transplant on someone Ed’s age, as the risks are too great,” Benedetti said. “With Lantidra, there are no surgical risks, and instead of being in the hospital for up to 12 days following an organ transplant, he was home within 24 hours.”
Milestones Lead to a Cure
This breakthrough has been long in the pipeline, but is now yielding positive effects, including restored insulin production, fewer life-threatening hypoglycemic episodes, and protection of kidney function and other vital organs. However, how long the remission lasts remains to be seen.
Though this can’t be considered a cure, it’s still a win for the diabetes community, showing that replacing beta cells can restore normal insulin production.
Researchers are developing multiple strategies to protect implanted insulin-producing cells, allowing patients to avoid lifelong immunosuppression. One approach is encapsulation (like Sernova’s CellPouch™), where donor or stem-cell-derived islets are placed inside biocompatible materials or devices that let glucose and insulin pass through but shield the cells from immune attack.
Another strategy focuses on immune therapies that retrain the body’s defenses to tolerate beta cells. For example, COUR Pharmaceuticals is testing a nanoparticle therapy (CNP-103) designed to “teach” the immune system not to target the key proteins that trigger type 1 diabetes. Together, these approaches aim to make cell-based cures safer and more widely accessible.
Visit the Islet Cell Transplant Program to learn more, or make a donation to this important research.


.webp)





.webp)
.jpg)

.jpeg)
.jpg)

.jpg)

.jpg)
.jpg)
.jpg)

.jpg)

.jpg)



.jpg)
.jpg)



.jpg)



.jpg)

.jpg)




.jpg)

.jpg)
.jpg)


.jpg)

.jpg)
.jpg)




.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)

.jpg)
.jpg)

.jpg)




.jpg)
.jpg)
.jpg)

.jpg)


.jpg)

















.jpg)




.jpg)







.webp)









.webp)