T1D Guide
T1D Strong News
Personal Stories
Resources
T1D Misdiagnosis
T1D Early Detection
Research/Clinical Trials
7 Tips to Maximize Savings this Year for Insulin and Diabetes Supplies
Whether you’re living with type 1 diabetes (T1D) or parenting a child with T1D, some of the least pleasant parts of managing the condition have nothing to do with blood sugar. The most triggering can be: ordering supplies, navigating insurance companies, and covering out-of-pocket expenses—diabetes is not a cheap disease.

Much like hearing, “There will be a cure in the next five years,” people with type 1 diabetes are also used to another promise: lowering the rising cost of insulin.
7 Ways to Take Control of Insulin and Diabetes Supply Costs
Whether you’re insured, underinsured, or uninsured, here are some ways to start strong this year and be proactive when ordering insulin and diabetes supplies.
1. Take advantage of current insulin price caps and programs
Many major insulin makers (Sanofi, Eli Lilly, Novo Nordisk) offer $35/month pricing on standard insulins to people in the U.S., through manufacturer programs. Also, patients can use Amazon Pharmacy to access discounted pricing, with manufacturer-sponsored coupons that bring the cost of many brands (Humalog, Novolog, and Lantus) down to $35/month.
Important Note: Through the Lilly Insulin Value Program, all Lilly insulins are available for $35 a month, regardless of whether you have commercial insurance or none.

Be sure to check with your pharmacy and ask them to apply available manufacturer copay cards or savings programs when you pick up insulin.
2. Use pharmacy discount tools
Prescription discount services like GoodRx, SingleCare, and ScriptSave WellRx can significantly reduce costs for insulin, test strips, glucometers, needles, and other essentials — often even below insurance copays for some people.
It’s worth comparing prices across pharmacies (including retail vs. mail order) before you fill.
3. Order supplies strategically
It typically pays to buy in bulk (hello Costco!) or use mail-order options. By ordering larger quantities (e.g., 90-day supplies) you can reduce the cost per unit, and these services often include free shipping.
Additionally, it’s a good idea to compare online suppliers and warehouse retailers. Some offer lower prices on strips or needles than traditional pharmacies. When buying online, always verify that products are legitimate and check expiration dates.

4. Explore patient assistance and nonprofit programs
Manufacturers and nonprofits offer assistance programs that can provide free or low-cost insulin and supplies if you qualify based on income or insurance status. In addition to Lilly Cares, Novo Nordisk offers the Novo Nordisk Patient Assistance Program, and Sanofi, the French pharma company, has expanded its $35/month insulin price cap to all U.S. patients, including those without insurance, on Medicare or covered by commercial plans.
Organizations like the American Diabetes Association (ADA) and community health centers can connect you with additional local resources and help you apply.
5. Use tax-advantaged accounts
Health Savings Accounts (HSAs) and Flexible Spending Accounts (FSAs) let you set aside pre-tax dollars for diabetes-related expenses, including insulin, supplies, copays, and deductibles, thereby reducing your overall expenses.
6. Work with your healthcare team
Ask your endocrinologist or health care team whether the less expensive (generic versions) are acceptable choices for your care. Make sure prescriptions meet your needs and that your insurance covers the full cost. Sometimes you have to get firm and demand more than they are willing to provide.
Remember, you’re probably speaking to an insurance agent who may not know how many test strips, infusion sets, or insulin vials fit your needs.
7. Don’t cut corners on care
It’s extra work, but don’t sacrifice your health to save money or reduce the care you need. You shouldn’t have to go without a sensor or test strips for even a few days. Monitoring tools help keep you healthy and reduce complications that are more costly over time.
Unfortunately, insulin and diabetes medication prices vary widely, depending on insurance status, manufacturer programs, and which state you live in. There’s no one-size-fits-all insulin therapy regimen.

Insulin Pricing in 2026- What the Future Holds
The good news is that, in 2026, insulin prices in the U.S. are expected to stabilize. Expected changes include the following:
Private Health Insurance (Employer Plans & Marketplace Plan)
There’s no federal law that universally caps insulin costs in the U.S. for all privately insured people yet, but:
- Some states have state-level caps on insulin copays for commercial insurance plans. For example, the ADA has applauded California's caps on insulin copayments at $35 per 30-day supply for many state-regulated health plans (effective 2026 for large groups, 2027 for small groups)
- Other states have their own caps (e.g., $25–$100), but there’s no nationwide cap on private insurance in 2026. Check here for a state-by-state overview of insulin copay caps.
- Without a cap, your out-of-pocket costs can vary depending on your plan’s tier, deductible status, and copay/coinsurance structure. This can sometimes exceed $35/month if you haven’t met your deductible or if your plan places insulin in a high-cost-sharing tier.
Manufacturer & Insurer Programs
The three major insulin makers (Sanofi, Novo Nordisk, and Lilly) have voluntary programs that set a $35-per-month list price for many insulin products for all U.S. patients, including those with commercial insurance. However, details can vary by brand and insurance plan.
Medicare (65+ and some disabled adults)
If you have Medicare Part D (prescription drug coverage) or Medicare Advantage, the monthly insulin cost-sharing cap is $35 or less. Because of the Inflation Reduction Act, Medicare plans must limit what you pay each month.

Patients Without Insurance (cash-pay)
More affordable insulin options are available, with costs ranging from $35 to $55 per month through manufacturer assistance programs or nonprofit producers such as Civica.
Civica Rx Insulin
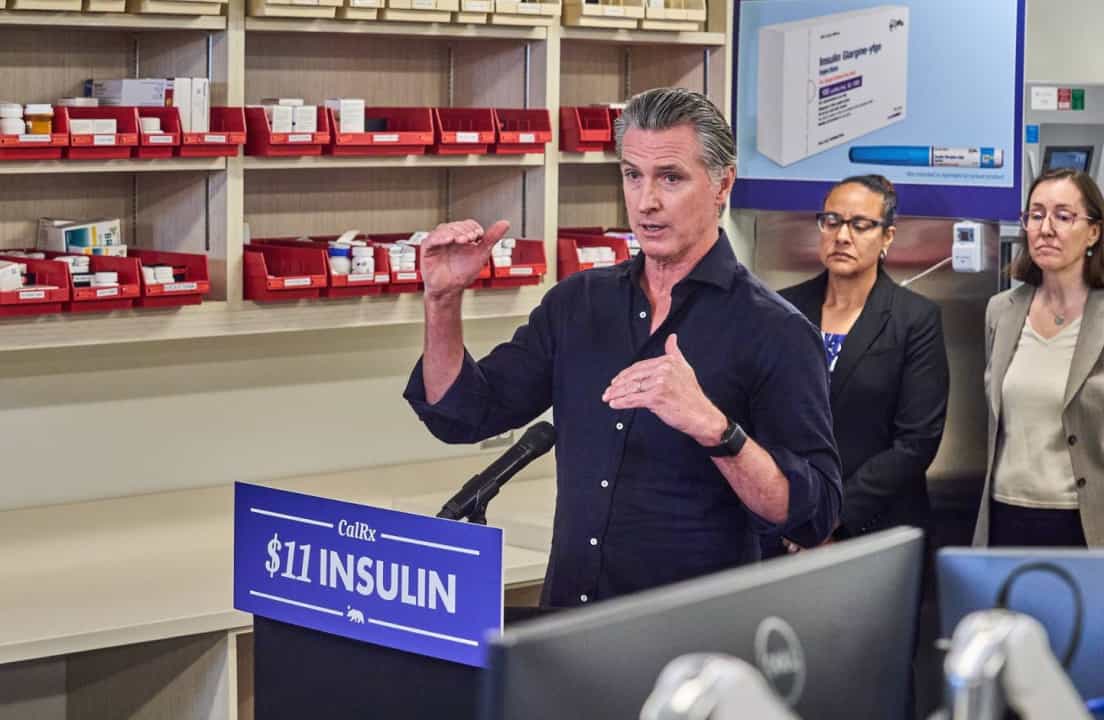
As of January 2026, the Golden State is the first in the country to partner with a nonprofit drug manufacturer, Civica RX, to develop, produce and sell its own insulin. Civica Rx is working with partners to make lower-cost insulins, including biosimilar or follow-on versions of common insulin types
CalRx is California’s state program that contracted with Civica Rx to produce and distribute affordable insulin under the CalRx brand name.
In an October press release, Governor Gavin Newsom said, “California didn’t wait for the pharmaceutical industry to do the right thing; we took matters into our own hands. No Californian should ever have to ration insulin or go into debt to stay alive.”
The suggested retail price for a vial of CalRx is:
- No more than $30 for a 10mL vial of insulin
- No more than $55 for a 5-pack of 3 mL pens
Blue Cross Blue Shield
What’s more, the Blue Cross Blue Shield Association (BCBSA) and many BCBS plans helped found CivicaScript, Civica’s outpatient-focused arm that works to bring lower-cost generic and biosimilar medicines to consumers.
New Year, New Savings
It may be a bit of extra work, but the key takeaway is to ask questions before you pay. Check your copay and insurance tier, and ask whether a direct-to-consumer cash price could save you money.
Remember, pharmacists are there to help. They can sometimes assist patients in exploring cheaper generics or similar alternatives, so you don’t get blindsided at the register.
To learn more information:
- CalRx website
- CalRx fact sheet
- ADA Center for Information
- T1International’s #insulin4all


.webp)





.webp)

.jpg)


.jpeg)
.jpg)
.jpg)

.jpg)
.jpg)
.jpg)
.jpg)

.jpg)

.jpg)
.jpg)



.jpg)



.jpg)




.jpg)

.jpg)



.jpg)

.jpg)




.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)

.jpg)
.jpg)

.jpg)



.jpg)
.jpg)
.jpg)

.jpg)

.jpg)














.jpg)


.jpg)







.webp)











.webp)









.webp)